A few weeks ago I wrote about a kind of cell that’s widespread through the body – fibroblasts, and their connection to erectile dysfunction. And now the fibroblast pops up again, this time in arthritis.
A groundbreaking study has, for the first time, uncovered the ability of joint fibroblasts to transition from causing inflammation to reducing inflammation in arthritis patients.
Led by an international team of researchers from Birmingham University and Germany’s Friedrich-Alexander University Erlangen-Nurnberg, it is a major step forward in understanding the complex interplay between fibroblasts, immune cells and resolving inflammation.
Fibroblasts populate the lining (synovium) of joints. Under healthy conditions, fibroblasts produce the lubricant that keeps the joints moving smoothly.
Birmingham Professor Adam Croft and his team have shown in disease conditions, fibroblasts can turn nasty, causing joint inflammation and damage in rheumatoid arthritis.
Importantly, however, fibroblasts aren’t targeted by any of the currently available treatments.
In this latest collaboration, however, the team has shown that these destructive fibroblasts can undergo an amazing switch to ones which instead promote the healing of joint inflammation.
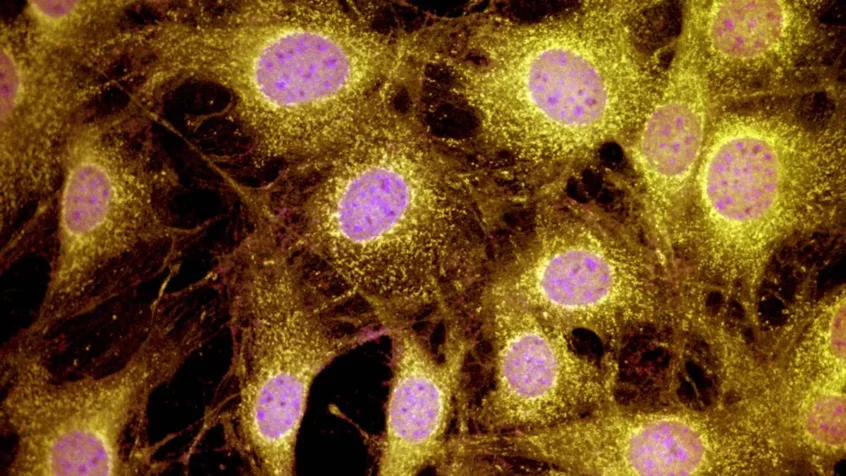
By using cutting-edge techniques to visualise and analyse fibroblast activity, researchers observed a reversal of fibroblast activity when inflammation was settling.
Further analysis revealed a switch in fibroblast types, from pro-inflammatory fibroblasts to pro-resolving fibroblasts. By looking inside human joints these pro-resolving fibroblasts were found clustering alongside anti-inflammatory lymphoid cells where the inflammation was resolving.
Professor Adam Croft, Versus Arthritis Professor of Rheumatology at Birmingham University, co-author of the paper, said: “This study shows for the first time that fibroblasts in the diseased joint can have both pathogenic and regulatory functions.
“We observed that resolution of joint inflammation was associated with a phenotypic switch from apathogenic to pro-resolving fibroblast phenotype that resulted in the stabilisation of specific immune cell populations that suppress inflammation.
“The next stage of this research is to develop therapeutic strategies to promote this switch in fibroblast phenotype in the joints of patients with arthritis. This would offer a novel therapeutic approach for those patients in which currently available drugs are ineffective.”
Lead author Professor Andreas Ramming, from the Friedrich-Alexander University Erlangen-Nürnberg, said: “Our research provides compelling evidence of a molecular shift within fibroblasts during the resolution of inflammation, with implications for understanding the pathogenesis of chronic inflammatory diseases like arthritis. By elucidating the mechanisms underlying fibroblast activation and resolution, we aim to identify new therapeutic targets for promoting inflammation resolution and tissue homeostasis.”
That is truly ground-breaking research.