Proton beam therapy is cutting-edge technology which will probably one day replace X-ray therapy for cancer.
At the moment there’s only one centre in the UK using it, the Christie Cancer Hospital in Manchester. A second is planned for UCL Hospital in London next year.
This has meant patients who require high-energy PBT have had to go abroad for treatment, even though PBT for rare eye tumours has been available on the NHS at Clatterbridge Cancer Centre on the Wirral for the last 30 years.
Since 2008, some 1,400 patients have gone to hospitals in the US and Europe under an NHS overseas programme which funds treatment, transport and accommodation.
When the two new £125million centres are fully up and running, each will treat up to 750 patients a year.

“Many of the patients we’ll be treating will be children, young people, and those with what could loosely be termed as rarer tumours,” says Ed Smith, who heads the Christie unit.
“I suspect in the next three or four years, all of those who would have gone overseas will be treated here.”
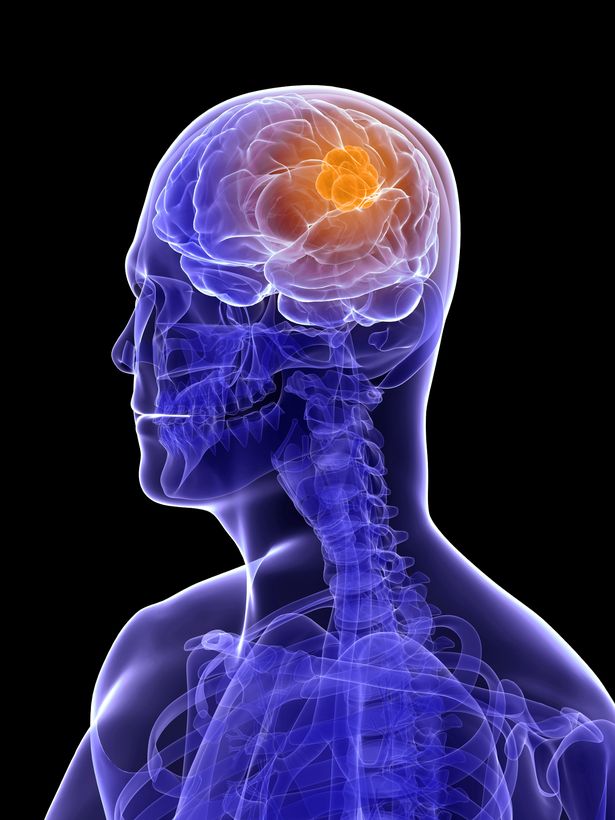
PBT is an advanced radiotherapy using a high-energy beam of protons, rather than the X-rays used in conventional radiotherapy.
Protons are aimed at the tumour and the beam stops once it hits the cancer cells, rather than carrying on through the body.
This means there’s little or no leakage into other tissues.
Conventional radiotherapy uses X-rays from multiple directions though a modern, high-precision variant aims to maximise the dose to the tumour while minimising its effect on the surrounding tissue.
However, the multiple beam still leaks into healthy tissue which receives substantial doses. PBT can provide important dose advantages compared with best quality X-rays.
In children and young adults, PBT could be used to treat some tumours in the brain, the head and neck area, and near the base of the skull or spine, as well as some soft tissue tumours and those in the pelvis.
In adults, tumours difficult to treat because they’re close to sensitive organs could benefit from PBT.
Chris Nutting, consultant clinical oncologist at the Royal Marsden Hospital, says repatriating patients from the overseas programme, and also treating those who might have been too unwell to be referred abroad, will be a success story.
I don’t think anyone would argue with that.
